![]()
In this episode, we are joined by Laura Legg, BESLER’s Director of Revenue Integrity Solutions, to discuss why DRG optimization efforts may be coming up short and what hospitals can do to improve reimbursement and compliance.
Podcast (hfppodcast): Play in new window | Download
Learn how to listen to The Hospital Finance Podcast on your mobile device.Most hospital leaders agree that DRG optimization is still an issue, despite current revenue cycle solutions.
A critical initiative is on the agenda at hospitals across the nation – revenue cycle optimization. From managing new provider payment models, finding and training staff on ever-changing documentation and coding requirements, to filling gaps in the patient experience, the thrust to improve the financial health of hospitals and acute-care facilities has never been greater.
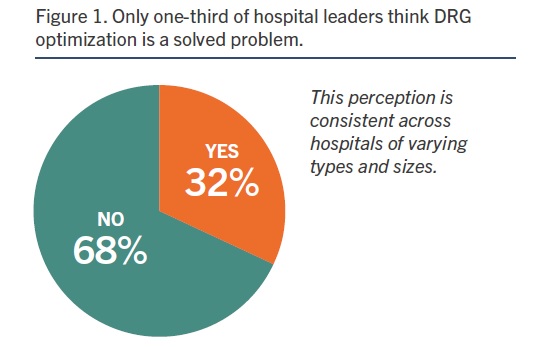
Opportunities for improvement abound. According to a recent HIMSS Media research study, Driving Optimal Revenue Cycle Performance, most of the nation’s hospital and acute-care facility leaders believe revenue cycle solutions are optimized for inpatient coding and audits (72 percent). Yet only one-third believe diagnosis-related group (DRG) optimization is a solved problem (Figure 1). As the DRG payment system marks its 36th anniversary, the complexity remains.
The HIMSS Media study also shows that nearly half of hospitals and acute-care facilities (47 percent) have established a revenue integrity program with three-fourths noting positive impact on:
- Net collections
- Gross revenue capture
- Reduced compliance risk
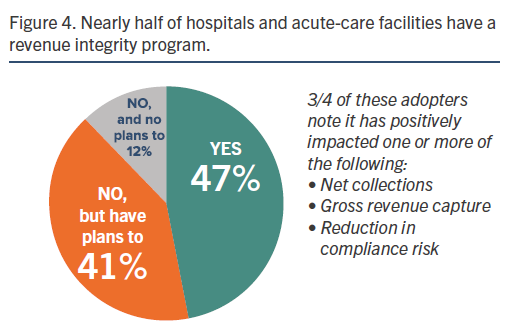
The more than 40 percent who don’t have a revenue integrity program have plans to deploy one (41 percent) (Figure 4).
Revenue integrity departments are addressing issues in a more proactive way than ever, according to Legg. “A good program goes across the entire revenue cycle, from patient registration and scheduling, to claim adjudication,” she said. “A good revenue integrity program can increase revenue and lower compliance risks, such as over-coding and having a higher DRG assignment and DRG relative weight than what the documentation in the patient record demonstrates.”
“The opportunity is there for hospitals to bring in the correct amount they are entitled to, and that can often be more than what the hospital has billed for,” said Legg. “Program staff need to look at all the functions and processes across the entire revenue cycle to ensure compliance and ensure processes are performed correctly so the end result is a clean claim.”
This episode of the Hospital Finance Podcast delves into DRG optimization including:
- Background on DRG optimization and how it’s changed over the past 30 years.
- What industry standards are used to determine DRGs during in-patient coding audits.
- Why DRG optimization is such an important issue for hospitals right now.
- Challenges hospitals face when looking to achieve DRG optimization.
The bottom line is this: With the right processes and third-party partner support, hospitals can help stop revenue loss and collect more of the money they deserve for the care they provide.
Episode Transcript: DRG optimization – still not a solved problem
Mike Passanante: Hi, this is Mike Passanante. And welcome back to the Hospital Finance Podcast.
Recently, BESLER released a white paper entitled Driving Optimal Revenue Cycle Performance. And that white paper details research that we and HIMSS Media conducted looking at over 100 respondents in revenue cycle and HIM and other areas of finance within the hospital about their perceptions of where revenue cycle is going right and perhaps where some things are going wrong.
One of the statistics that stood out to us during that research were that one-third of the respondents felt that DRG optimization was a solved problem. And that, given that many of them felt that their software was optimized to handle DRGs appropriately.
And so, we kind of want to sort that out for you here today. And to join me in walking through that topic is Laura Legg who’s our Director of Revenue Integrity Solutions at BESLER.
Welcome to the show, Laura.
Laura Legg: Thanks Mike. And thank you for having me.
Mike: A pleasure as always.
Laura, for those in our audience who are not familiar with the term DRG optimization or what that’s all about, could you just explain that for us?
Laura: Sure, Mike. Understanding DRG optimization does require a little bit of background.
The important parts are DRGs were developed at Yale University in the late 1960s. But they were developed to monitor quality of care and utilization of services for hospitals and patients. So, they really served as part of cataloging patient diseases and conditions.
But all that changed in the 1980s when it was changed to a means for determining hospital reimbursement for in-patient stays in the United States. It’s important to note that we are the only nation in the world that uses DRGs as a reimbursement methodology.
DRG optimization is a term used by hospitals that’s striving to obtain optimal reimbursement or the highest possible payment to which the facility is legally entitled based on the coded data supported by clinical documentation in the patient’s record.
It kind of goes back, Mike, to that old saying “if it was not documented, it was not done.” So if a hospital performs services, and they aren’t documented, the payment for those services can be denied.
People do use a lot of different terminologies when they’re talking about DRG optimization. They might use some interchangeable terms such as DRG validation or DRG audits. But that’s really where DRGs came from just a little background, Mike.
Mike: Great! Thanks for that Laura. Laura, can all hospitals optimize DRGs?
Laura: Yes, Mike. Hospitals that are reimbursed using the DRG system should be optimizing their DRGs to ensure optimal revenue capture. Not doing so could be a significant loss in revenue.
Critical access hospitals are exempt because they’re paid a percentage of their target and not paid by DRGs.
So, when you’re a hospital that’s doing DRG optimization, Mike, it’s important to point out that they also need to be ensuring compliance for the regulatory requirements around DRGs. And those regulatory requirements are set by CMS, the OIG and some other entities.
So, it’s really important to know that any good DRG optimization endeavor also includes a review of the claims for compliance which means you’re reviewing DRG payments that might exceed the correct amount.
So, both DRG optimization and compliance reviews are complex processes but they’re equally important. Medicare does not want claims to be over-coded or under-coded. Medicare wants hospital plans to be submitted with the correct DRG assignment.
Mike: So, let’s get into how DRG optimization is done. Can you explain that for us?
Laura: DRG optimization, Mike, is done through in-patient coding audits. An organization should audit all the elements on an in-patient claim that are used to determine the DRG. And those are diagnoses, procedures and discharge status codes.
There are trained individuals and organizations sometimes that are certified coders that are experienced in ICD-10 code assignment. And those people can perform DRG optimization and compliance reviews.
Now, the main goal of these reviews is to verify the accuracy of the hospital’s diagnosis and procedure code assignment that affect DRGs. So really, in general, their job is to ensure the diagnostic and procedural information and the beneficiaries’ discharge status are coded and reported by the hospital on its claim and that those codes match both the attending physician’s description and the medical record documentation.
So, those coding experts really validate the principal diagnosis, secondary diagnoses codes, procedure codes. All that potentially can affect the DRG assignment.
Now, the actual process itself, Mike, is based upon the accepted principles of coding practice. So those are really industry standards. And the two most important references we have for that are—the CMS and cooperating parties publish what we call The Official Guidelines for Coding & Reporting. We also have the American Hospital Association that publishes Coding Clinic.
So, those are the two resources that should be used when organizations are reviewing for DRG validation.
Mike: And Laura, can you describe the optimization process after the DRG is assigned?
Laura: I can, Mike. And what it really is a second set of expert eyes to assure that all the coding is done according to industry guidelines and is consistent with the provider’s documentation in the record.
So, doing the DRG review process, it can be either pre-bill or post-bill. A difference in the initial DRG assignment and the reviewer’s DRG assignment may be found. When this happens, then a reconciliation process takes place.
When the final DRG assignment is determined, the claim is sent to the payer.
Traditionally, most DRG differences are ascribed to maybe a coding error implying that the established guidance from the Official Coding Guidelines and the AHA Coding Clinic were not followed. But there can also be a change in the sequencing of diagnosis or procedure codes that can change the DRG.
Well, once the final DRG assignment is made, the reconciliation takes place, the claim can then be billed or re-billed.
Mike: So Laura, hearkening back to my comments at the beginning of the podcast where most of the respondents, two-thirds in fact of the survey that was conducted, noted that the DRG optimization is not a solved problem. Why is this issue so important right now?
Laura: Well, one of the reasons, Mike, and probably the big reason, is that code assignment is done in one of the most vulnerable areas of revenue cycle—and that is coding and clinical documentation.
So, the coding aspect of it is especially vulnerable right now because we’re in a relatively new coding system, ICD-10. The previous industry accuracy rates under ICD-9 were about 95%. But last year, our ICD-10 accuracy rate was at about 57% nationwide. So that just tells you there is a lot of room for improvement.
Also contributing to that is the ICD-10 coding system updates yearly that change DRGs every year. And it makes it challenging for coders to keep up their knowledge base and maintain that high accuracy rate.
But really, what I can’t stress enough, Mike, is the importance of clinical documentation that’s accurate, complete, compliant and timely. Really, the documentation is the most important key to accurate coding and DRG assignment.
With the new specific codes in ICD-10, they’re all great. But if the provider documentation is not specific enough to the current code assignment, then you’re in trouble.
Mike: Okay! Laura, what are some of the challenges for hospitals that are looking to do DRG optimization?
Laura: Well, often, I hear, Mike—and it’s true—that DRG optimization does require resources because you’ve got to have the staff and the time to put into the actual process itself.
And that’s why leveraging your revenue cycle vendor is one option that can really lighten the load and the expense of DRG validation.
The days of manual coding audits are behind us. And there’s new technology in place today that allows hospital to look at hundreds of claims and analyze them in just a few minutes. And really that comes from the premise, Mike, that for a long time, for several years, we’ve known that RAC auditors and other payer auditors were able to review hundreds of records in a few minutes. So now, hospitals can also do that which kind of levels the playing field.
The claims that are flagged can then be fallout for further review and be looked at by an experienced coding analyst.
So, there’s many benefits to it including timeliness, the volume that you can review. And it also causes a reduction in claim denials.
The other I think real challenge is hospitals are so busy right now. There’s competing priorities. The challenge was all the initiatives that hospitals have going on, be it improvement activities, be it EMR updates. But DRG optimization can actually help offset the cost of some of these initiatives. So, it is a win in the eyes of hospital finance leaders.
Mike: Indeed! And I’m wondering if you can expand on that and talk about some of the additional advantages that hospitals can achieve when they engage in DRG optimization.
Laura: Well, Mike, besides the obvious increase in revenue that’s found during DRG optimization, there’s a compliance assurance of knowing that you’ve had a really strong double check system for your revenue integrity.
Also, when reviewing in-patient claims for DRG optimization, hospitals can take advantage of the workflow by including a review of other compliance and regulatory issues.
So, some of the things that can be worked in to the workflow of DRG optimization is a look at medical necessity, a look at quality measures, hospital-acquired conditions. And that’s really just naming a few.
So, these benefits really multiply the benefits of DRG optimization and ultimately results in better coding, better clinical documentation and cleaner claims.
Mike: Great detail there, Laura. And for those in our audience who might like to get a look at the research report that we’ve talked about here today, or the white paper itself, just head on over to Besler.com/insights. You can click on the revenue integrity tab that you see there on the page. That will take you to an area where you can get to all of those resources.
Laura, thank you so much for joining us on the podcast today.
Laura: You’re welcome, Mike. Thank you.





